Conditions
Plantar Fasciitis
Plantar Fasciitis Treatment in Chilliwack
Plantar fasciitis is one of the most common types of persistent foot pain, especially around the heel. Our plantar fascia is a connective tissue structure that attaches from our heel to the base of our toes. It’s function is to help support the arch, aid in propulsion during normal gait, and help with shock absorption by distributing force across the foot.
When the plantar fascia is overworked, small tears can occur leading to a repetitive cycle of inflammation and adaptive thickening. As this happens, the insertion point of the plantar fascia on the heel can start to get inflamed and irritated, causing pain and difficulty walking or running. In textbook plantar fasciitis, pain is often worst when taking first steps after a period of rest (getting up in the morning, getting up after sitting for a while). Initially the heel pain improves as we get moving, but when allowed to progress, the pain can start to creep into the rest of our day.
There are a few short-term relief options for helping the plantar fascia, ranging in effectiveness depending on the person and the modality. These treatments are helpful to provide some initial relief, but can sometimes fall short at providing long-term improvements unless they are repeated. This is part of why plantar fasciitis is known to be such a stubborn condition.
For more long-term relief, it’s more effective to consider how your overall foot mechanics place added stress on the plantar fascia tissue. By identifying risk factors that place more force or load on the plantar fascia, we can find ways to then offload or reduce the stress placed on the plantar fascia in standing, walking, and running. For example, weak intrinsic foot muscles, excessively tight calf muscles, too high or too low of an arch, and poor big toe function are just some of the mechanical risk factors that increase the stress on the plantar fascia. For many people, assessing foot function and seeing if there are any mechanical reasons that keep irritating the plantar fascia is the key to long-term relief and management.
See below for treatment options & causes of plantar fasciitis as well as other types of heel pain.
Causes of Plantar Fasciitis
Below are some of the most common causes of added strain on the plantar fascia that can contribute to plantar fasciitis.
-
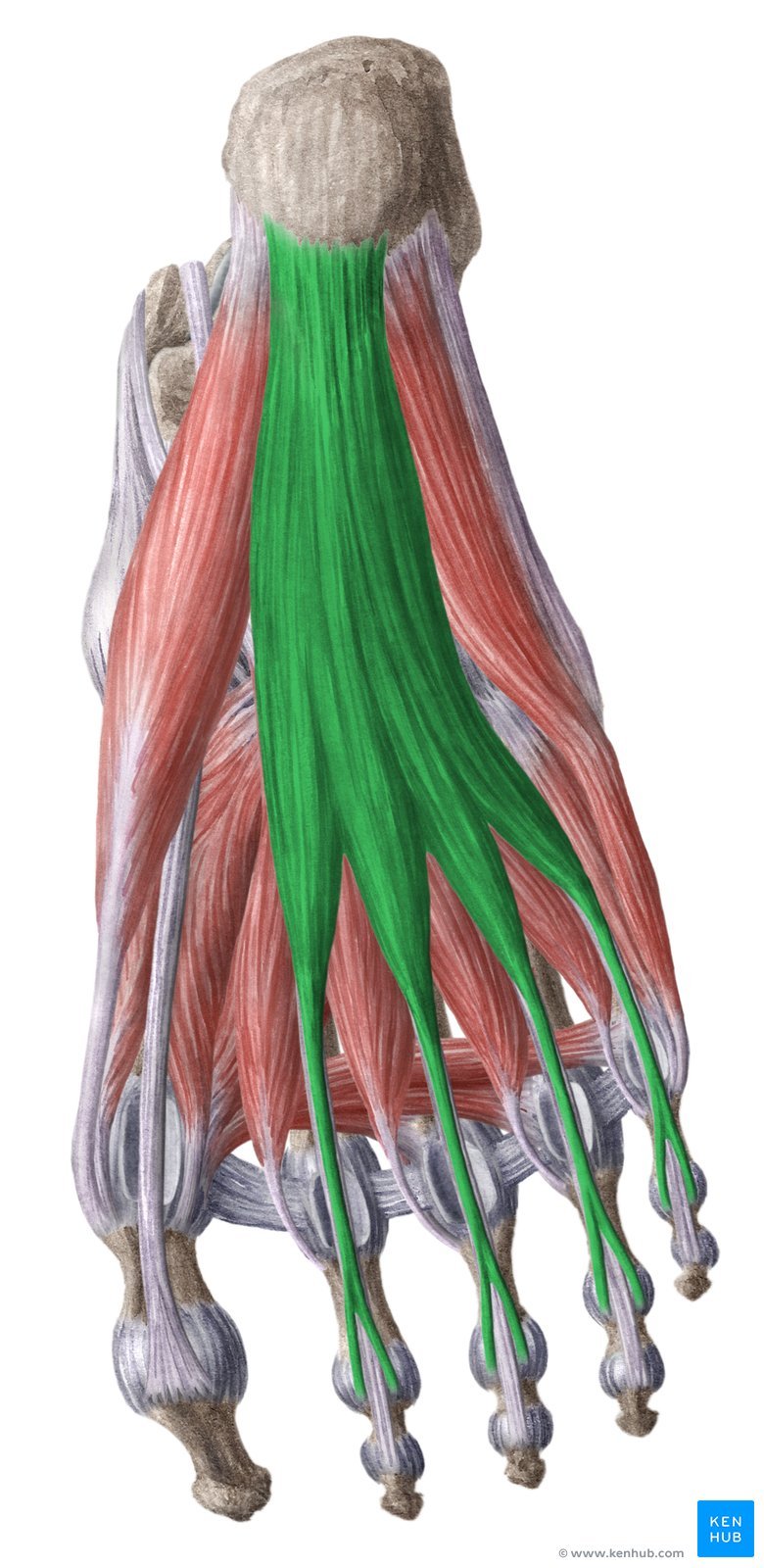
Weakness in one or more of the muscles of the feet is a major contributor to adding stress on the plantar fascia.
This is an issue that happens slowly over time, often due to lack of activity, a specific foot function problem, or wearing over-supportive footwear.
As a result, examining the most important foot muscles that take pressure of the plantar fascia is a very important part of plantar fasciitis treatment for long-lasting results.
-
Having our inner foot arch be too high or too low (there is a normal range) can effect plantar fasciitis. This usually happens directly by adding additional pull force from the plantar fascia onto the heel when we stand or walk (in the case of an arch too low), as well as by compromising other foot functions such as shock absorption and force dampening. In this situation a custom orthotic can be a very helpful part of treatment to hold the arch in a neutral position and improve shock absorption at the foot.
For example, rearfoot valgus (shown below) involves bowing in of the heel and a lower than normal arch. This adds to increased pull on the plantar fascia. A custom orthotic in this case places the arch and heel in a neutral position, allowing for proper foot mechanics and decreased repetitive strain on the plantar fascia, leading to a reduction in plantar fasciitis symptoms.
-
There are certain styles of running or walking that can amplify forces on the plantar fascia. In walking if someone overpronates (ankle rolls inward too much, often with a low arch) it can lead to an extra pull on the plantar fascia. In running, when we run with a forefoot strike pattern we place additional strain on our “posterior chain”. This includes the calf, achilles, and plantar fascia.
If abnormal walking or running mechanics is found to be a major contributor, then using walking or running modifications to distribute forces is very effective. This is usually best examined through a gait exam in the office.
-
Like the above issues, weakness in our ankle muscles lead to altered foot mechanics that can in turn add stress and strain to the plantar fascia tissue.
This is common for people after repetitive ankle trauma such as sprains or strains. If this is a cause, then re-strengthening these muscles becomes an important part of treating the plantar fascia.
-
A flexible and strong big toe joint is one of the most important parts of healthy foot function. Our big toe acts to propel our momentum forward when walking, and the muscle underneath it is one of the biggest contibutors to holding up a healthy arch.
Conditions such as big toe arthritis or turf toe add additional pressure on the plantar fascia by reducing big toe range of motion and strength.
In these cases, working on improving big toe mechanics becomes very helpful to treating the plantar fasciitis. Additionally, finding proper footwear to allow for healthy big toe function is also important.
Rearfoot valgus involves bowing inward of the heel and back of the foot. This is one of many foot function issues that can lead to added stress on the plantar fascia over time, in this case by causing an excessively low arch that leads to a stronger pull on the heel bone from the plantar fascia.
Other Causes of Heel Pain
When it’s not plantar fasciitis. There are other tissues that attach in and around the same area as the plantar fascia, that can mimic plantar fasciitis and often be misdiagnosed as plantar fasciitis. Below are the most common ones.
-
Tibialis posterior is a muscle that runs along the inside of our lower leg and attaches to our inner foot, just past the heel. Issues with this muscle can sometimes cause pain to refer to the inner heel, thereby mimicking plantar fasciitis.
In some cases weakness of the tibialis posterior muscle can also contribute to plantar fasciitis by adding extra force to the plantar fascia when walking or standing.
-
The medial plantar nerve branches off of the posterior tibial nerve, then supplies sensation to the area as well as strength to some of the foot muscles.
If the nerve is compressed along it’s course down the lower inner leg and foot, it can cause pain and weakness in the area of the inner heel, thereby mimicking plantar fasciitis.
There are many cases of plantar nerve entrapment that are misdiagnosed as plantar fasciitis because of this location overlap. A good physical exam where we check for nerve sensitivity in the posterior tibial nerve and the medial plantar nerve will help to differentiate this from a plantar fasciitis issue.
-
Baxter’s neuropathy involves compression of the inferior calcaneal nerve that supplies sensation to the inner heel.
The nerve arises similarly as the plantar nerve, but more often gets compressed by one of the big toe muscles, the abductor hallicus.
Compression of this nerve causes inner heel pain, thereby mimicking plantar fasciitis.
-
There are a few muscles that attach around the plantar fascia, either deep to it or beside it.
The tendons (the portion of the muscle that attaches to the bone) of these muscles can get injured or irritated, causing tendinitis or tendinosis. Flexor digitorum brevis is a muscle that is often involved with plantar fasciitis, either because it is weak and leads to increased force on the plantar fascia, or because its tendon is directly inflamed and is mimicking plantar fasciitis.
As a result, flexor digitorum tendon issues are often misdiagnosed as plantar fasciitis.
A common cause of heel pain besides plantar fasciitis. Flexor digitorum brevis is a muscle that lives one layer deep to the plantar fascia. Weakness in this muscle is a common contributor to true plantar fasciitis, and tendinitis of this muscles tendon at the heel can mimic plantar fasciitis.